Vaccination
In 1768 John Fewster an English Physician realised that prior infection with cowpox rendered a person immune to smallpox DOI. However it was not until 1796 Edward Jenner, postualted that the pus in cowpox blisters protected the individuals from smallpox. Jenner took pus from blisters on the hands of Sara Nelmes and inoculated James Phipps (an 8 year old gardeners son) who developed a mild fever. Subsequent exposure to smallpox material did not elicit any sign of infection. More details of this first recorded vaccination are available at The Edward Jenner Museum.
Smallpox is a highly contagious and once inhaled the virus invades mucous membranes and from there to lymph nodes, around 12 days after infection there is considerable cell lysis and high levels of virus can be found in the bloodstream. Mortality is around 30% and is higher in children. Over the years smallpox has been estimated to have killed hundreds of millions of people WHO.
Mandatory smallpox vaccination came into effect in Britain and parts of the United States of America in the mid 1800s and In 1958, the World Health Assembly called for the global eradication of smallpox by worldwide vaccination. In 1980 smallpox was officially eradicated saving millions of lives.
How do vaccines work?
Our immune system has a fantastic ability to protect against disease, it can detect a huge variety of pathogens such as virus and bacteria. The innate imune system provides a rapid but non-specific response, humans like all vertebrates have a second layer of defence called the adaptive immune system, this system adapts the response through improvement of recognition of the pathogen. When the immune system first meets a virus it hasn’t seen before, the amount of antibody and the number of T-cells that recognise it are very low. It usually takes around a week for enough to be produced to mount an effective immune response. This then results in an immunological memory allowing the adaptive immune system to respond faster and more effectively to subsequent exposure. This fine-tuning of the adaptive immune system takes about a week and for some pathogens the damage is done before the immune response can be mounted.
Vaccines harness the our natural adaptive immune system, the vaccine primes the adaptive immune system by exposure to an agent (an immunogen). The immunogen could be a related but harmless agent as in the case of cowpox protecting against smallpox, or it could be an attenuated virus (created by reducing the virulence of a pathogen, but still keeping it viable) or an inactivated virus (killed virus). Ideally the vaccination occurs before exposure to the pathogen so the adaptive immune system is able to refine the recognition of the immunogen and thus mount an immediate response.
Adjuvants
An adjuvant is a substance that increases or modulates the immune response to a vaccine, in the initial production of vaccines it was observed that some contaminants actually improved the efficacy of vaccines. Subsequent work showed that so called pathogen-associated molecular patterns, which include liposomes, lipopolysaccharide, molecular cages for antigens, components of bacterial cell walls, and endocytosed nucleic acids such as RNA, double-stranded RNA, single-stranded DNA, and unmethylated CpG dinucleotide-containing DNA that the immune response already knows about can enhance the immune response. DOI.
RNA vaccines
Vaccines work by identifying part of the virus as foreign, this could part of the viral coat protein, so in theory we only need to introduce the viral coat protein for the adaptive immune response to recognise it and be activated. Messenger RNA (mRNA) vaccines work by introducing a piece of mRNA that codes for a viral specific protein, usually a small piece of a protein found on the virus’s outer membrane. The host cell can then use this mRNA as a blueprint to build the viral protein. As part of a normal immune response, the immune system recognises that the protein is foreign and produces specialised proteins called antibodies. Because the mRNA introduces only a single protein (a virus is made up of many proteins) there is no risk of a viral infection.
Whilst mRNA vaccines have received considerable attention due to their use during the COVID pandemic, the research around this technology has been around for many years, with the first experiments published in 1989 DOI. The development of the COVID vaccines were accelerated because a number of the safety studies were done in parallel rather than sequentially, normally the costs and resources would not have allowed this. Manufacturing was started at risk even before regulatory approval.
The mRNA is rapidly degraded in the cytosol and has to be stored at low temperatures. Whilst retroviruses like SARS-Cov-2 have mechanisms to enter the cell nucleus and reverse transcriptase and appropriate primers to make DNA from the RNA in the cell nucleus, mRNA vaccines lack all these mechanisms and can't be converted to DNA.
How are they tested
Most of the initial work is done in cells in specially built biosafety labs, subsequently the vaccine will be tested in small animals usually mice. Subsequent safety studies are conducted, these are more rigorous than most drug safety studies because vaccines are to be given to a large population of healthy individuals many of whom may be children. We can perhaps contrast this with some drugs used to treat cancer, these drugs are designed to kill cells, and by their nature there is likely to be some toxicity.
Sometimes, a ‘controlled human infection model’ (CHIM) is used to help the development of a vaccine. This type of carefully controlled study is where a healthy, fully consenting volunteer is deliberately infected with a disease, usually to test how well the vaccine works. The volunteer is then monitored very closely, and if they become symptomatic, they are offered an effective treatment.
What vaccines are available?
The WHO lists 25 different diseases that can be vaccinated against, with another 16 in development. For some diseases there may be multiple vaccines available, in addition some are given in combination e.g. MMR (measles, mumps and rubella) vaccine DOI.
Cholera
COVID-19 (corona virus)
Dengue
Diphtheria
Hepatitis
Haemophilus influenzae type b (Hib)
Human papillomavirus (HPV)
Influenza
Japanese encephalitis
Malaria
Measles
Meningococcal meningitis
Mumps
Pertussis
Pneumococcal disease
Poliomyelitis
Rabies
Rotavirus
Rubella
Tetanus
Tick-borne encephalitis
Tuberculosis
Typhoid
Varicella
Yellow Fever
For some pathogens developing a vaccine is proving challenging, the common cold can be caused by a large number of different viruses so a single vaccine would have very limited efficacy. The flu virus constantly mutates and so a new vaccine is needed each year activate against the strain that is predicted to be dominant during the flu season.
Do vaccines work?
They clearly do, the eradication of smallpox is a great example of how effective vaccination can be, before the vaccine 1 in 3 infected died.
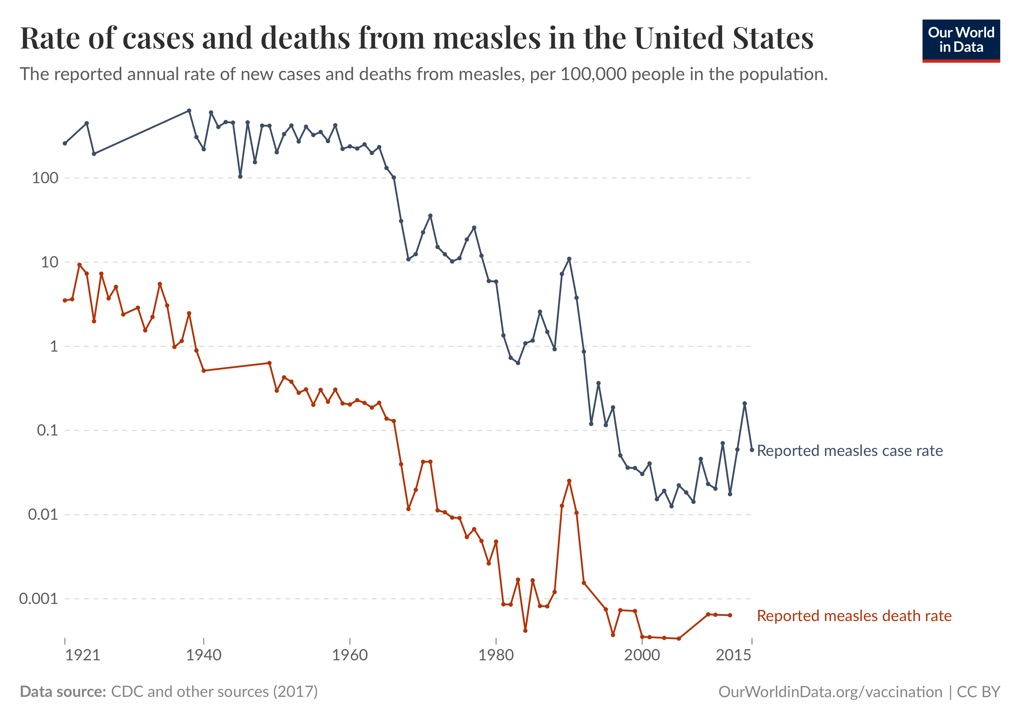
Measles used to be common in the USA, after vaccination in the 1960s cases and deaths dropped.
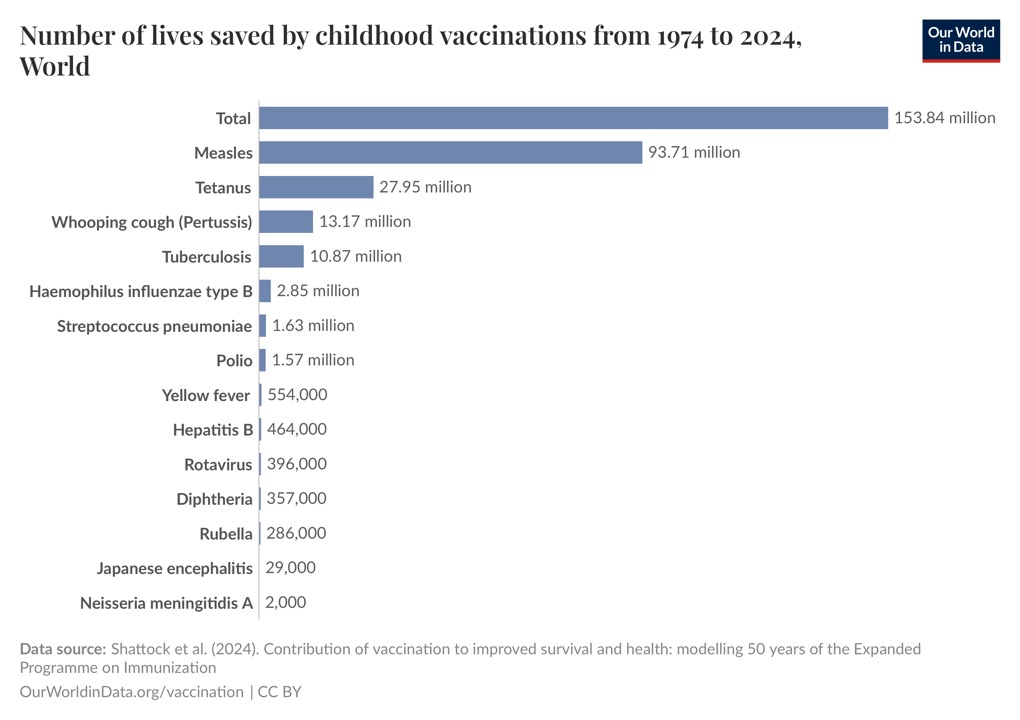
It is difficult to estimate the number of lives saved by vaccines but the Our World in Data site does give us an idea of the staggering number of lives saved.
It is worth remembering that virus infections can result in long-term issues. Cervical cancer is the fourth-most common cancer in women worldwide, and nearly all cervical cancers are caused by an infection with certain high-risk types of human papillomavirus (HPV). HPV vaccination has been show to prevent cervical in those vaccinated, a recent study DOI found no cases of invasive cancer were recorded in women immunized at 12 or 13 years of age. Several other studies have recorded similar results DOI. Many other cancers are thought to be caused by HPV DOI.
Some concerns and the evidence
Vaccines are not associated with autism or developmental delays DOI
A meta-analysis review of 10 studies (5 cohort and 5 case-control involving over 1.25 million children looked at autism spectrum disorders (ASD), vaccines, the ingredient thimerosal (mercury) and the measles-mumps-rubella (MMR) vaccine. No causal association was found between vaccinations and ASD or between ASD and the MMR vaccine, specifically. In addition, no causal association was found between ASD and thimerosal.
Also Increasing Exposure to Antibody-Stimulating Proteins and Polysaccharides in Vaccines Is Not Associated with Risk of Autism DOI00144-3/fulltext)
Autism Occurrence by MMR Vaccine Status Among U.S. Children With Older Siblings With and Without Autism DOI.
The MMR vaccine was not associated with increased risk of ASD, regardless of whether older siblings had ASD. These findings indicate no harmful association between MMR vaccine receipt and ASD even among children already at higher risk for ASD.
Relationship between MMR vaccine and autism DOI.
Based upon the current literature, it appears that there is no relationship between MMR vaccination and the development of autism.
Worth reading
How the case against the MMR vaccine was fixed DOI.
Brian Deer exposes the bogus data behind claims that launched a worldwide scare over the measles, mumps, and rubella vaccine, and reveals how the appearance of a link with autism was manufactured at a London medical school.